Menu

Articles
Practice announcements and news about neurosurgical research and educational meetings.

Featured
Practice Updates
Merry Christmas and a Happy New Year
Wishing all out Patients and Referrers a Happy Christmas and Peaceful new Year
Featured
Events
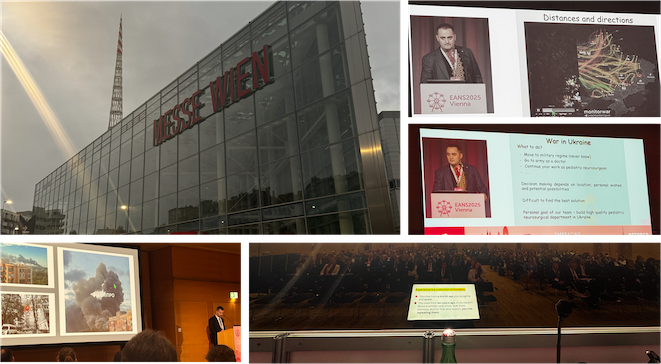
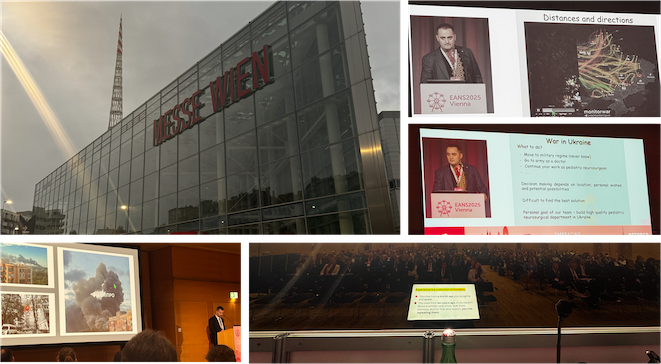
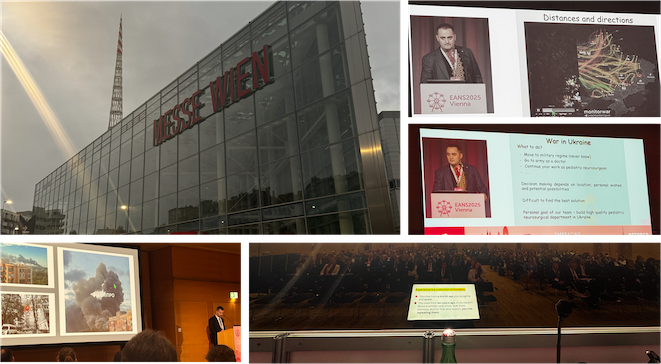
European Association of Neurosurgical Societies Annual Congress, Vienna, 2025.
Neurosurgeons from across the world gathered in Vienna in October 2025 for the Congress of the EANS.

Featured
News
Professor M. Gazi Yasargil (1925-2025)
The passing of Professor Yasargil was announced by the Turkish Health Ministry this morning.

Featured
Events
EU-Japanese Neurovascular Surgical Meeting, Vienna, 2024
Every two years experts in cerebrovascular surgery from Japan and Europe convene to share their unique perspectives and experiences.

Featured
News
Lecture tour to China 2024- Chongqing
The lecture tour of China continues to Chongqing, one of China's largest cities.

Featured
Events
Lecture tour to China 2024- Lianyungang
A visit to the neurosurgery department at the First People's Hospital of Lianyungang, Jiangsu province, China

Featured
Events
Royal Hospital Chelsea Founders Day
Chelsea Pensioners Founders Day Celebrations, 2024.
Featured
Events
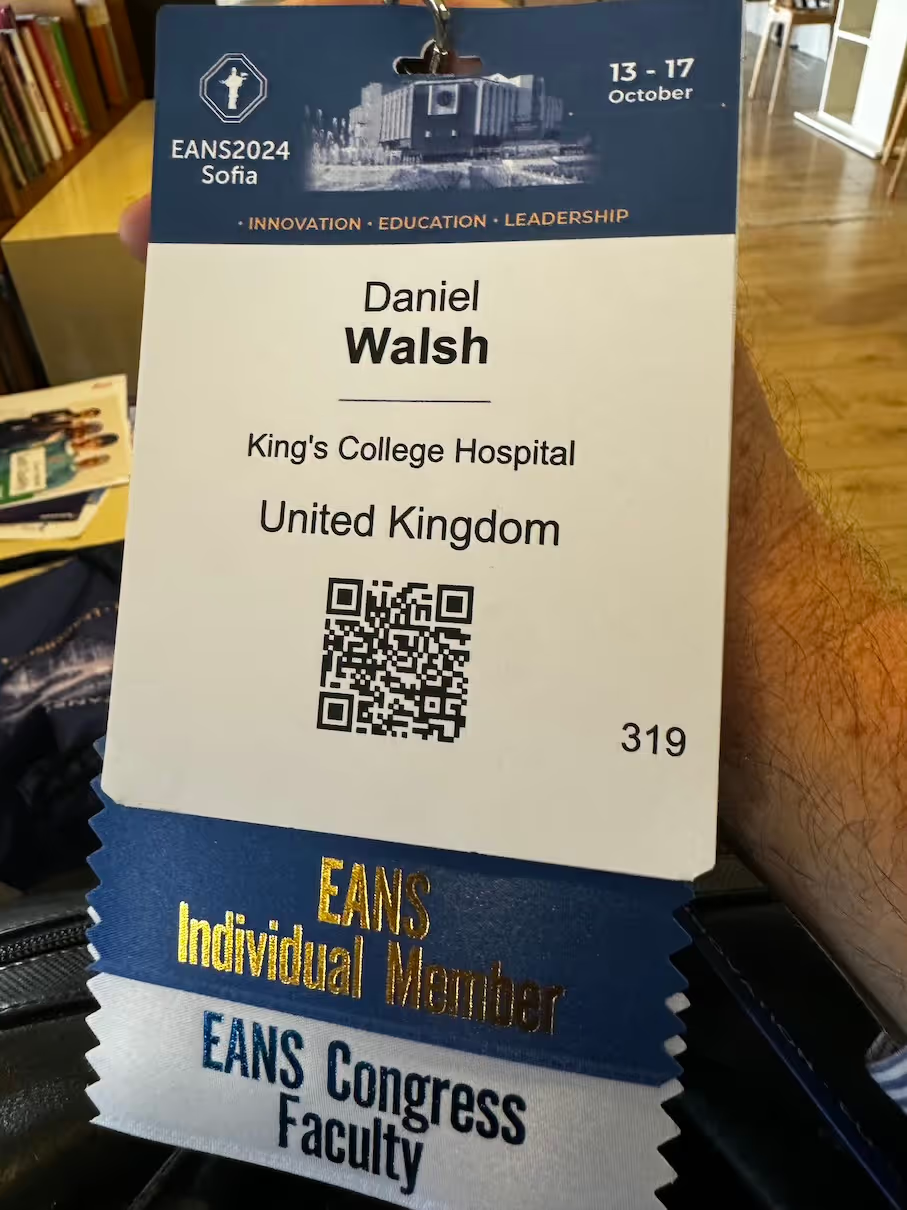
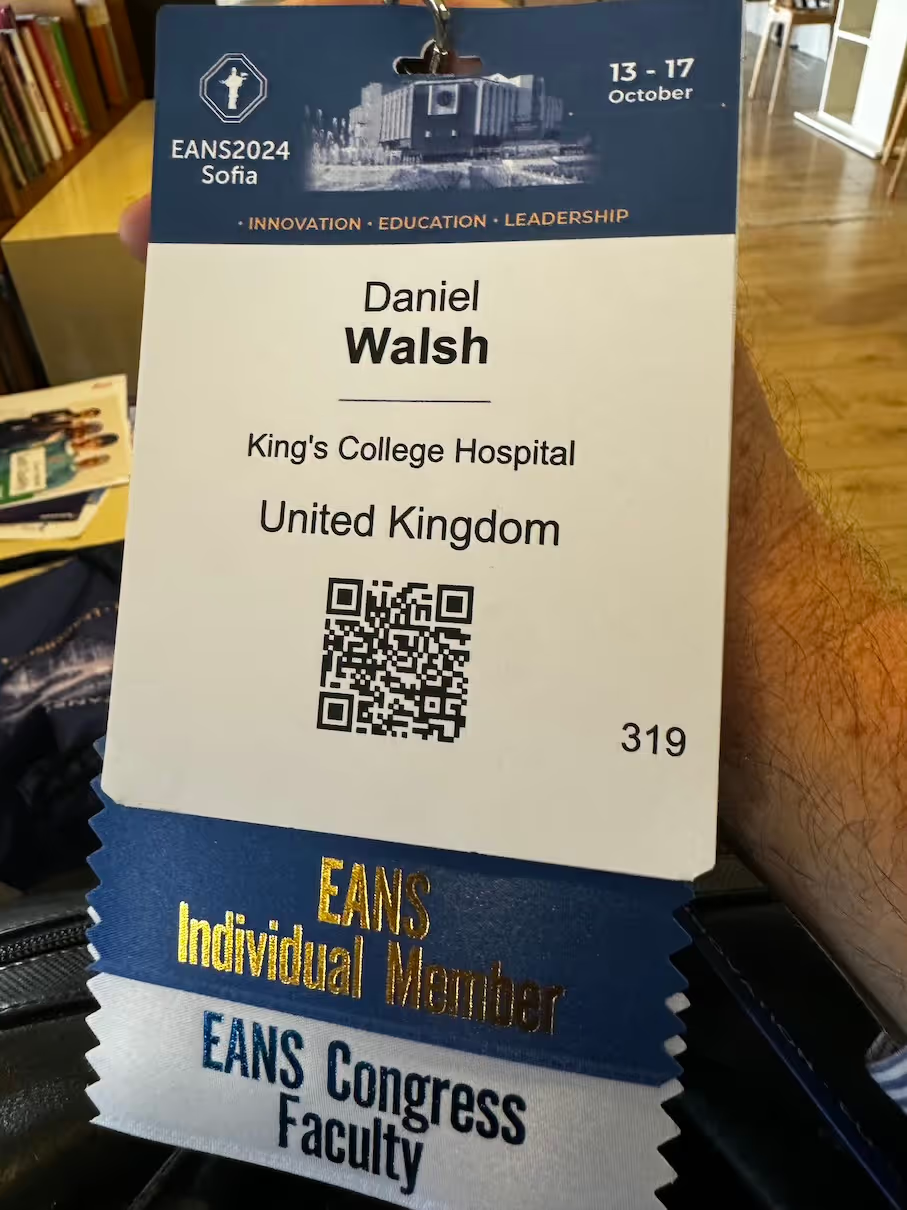
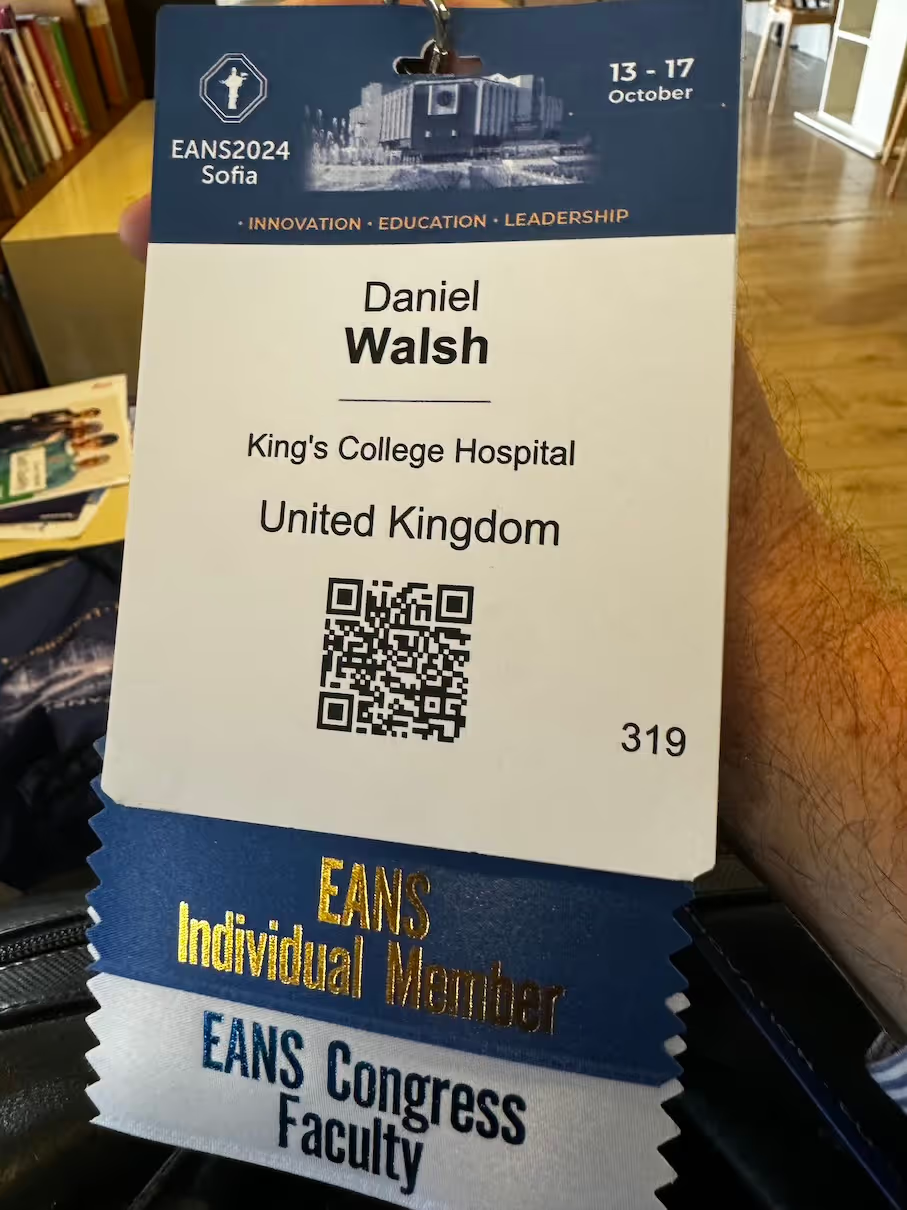
European Association of Neurosurgical Societies Congress 2024
Annual Congress of The European Association of Neurosurgical Societies

Featured
Practice Updates
Merry Christmas and a Happy New Year
Wishing all out Patients and Referrers a Happy Christmas and Peaceful new Year
Featured
Events
European Association of Neurosurgical Societies Annual Congress, Vienna, 2025.
Neurosurgeons from across the world gathered in Vienna in October 2025 for the Congress of the EANS.

Featured
News
Professor M. Gazi Yasargil (1925-2025)
The passing of Professor Yasargil was announced by the Turkish Health Ministry this morning.

Featured
Events
EU-Japanese Neurovascular Surgical Meeting, Vienna, 2024
Every two years experts in cerebrovascular surgery from Japan and Europe convene to share their unique perspectives and experiences.

Featured
News
Lecture tour to China 2024- Chongqing
The lecture tour of China continues to Chongqing, one of China's largest cities.

Featured
Events
Lecture tour to China 2024- Lianyungang
A visit to the neurosurgery department at the First People's Hospital of Lianyungang, Jiangsu province, China

Featured
Events
Royal Hospital Chelsea Founders Day
Chelsea Pensioners Founders Day Celebrations, 2024.
Featured
Events
European Association of Neurosurgical Societies Congress 2024
Annual Congress of The European Association of Neurosurgical Societies

Featured
Practice Updates
Merry Christmas and a Happy New Year
Wishing all out Patients and Referrers a Happy Christmas and Peaceful new Year
Featured
Events
European Association of Neurosurgical Societies Annual Congress, Vienna, 2025.
Neurosurgeons from across the world gathered in Vienna in October 2025 for the Congress of the EANS.

Featured
News
Professor M. Gazi Yasargil (1925-2025)
The passing of Professor Yasargil was announced by the Turkish Health Ministry this morning.

Featured
Events
EU-Japanese Neurovascular Surgical Meeting, Vienna, 2024
Every two years experts in cerebrovascular surgery from Japan and Europe convene to share their unique perspectives and experiences.

Featured
News
Lecture tour to China 2024- Chongqing
The lecture tour of China continues to Chongqing, one of China's largest cities.

Featured
Events
Lecture tour to China 2024- Lianyungang
A visit to the neurosurgery department at the First People's Hospital of Lianyungang, Jiangsu province, China

Featured
Events
Royal Hospital Chelsea Founders Day
Chelsea Pensioners Founders Day Celebrations, 2024.
Featured
Events
European Association of Neurosurgical Societies Congress 2024
Annual Congress of The European Association of Neurosurgical Societies